Hello world!
Welcome to WordPress. This is your first post. Edit or delete it, then start writing!
We recommend no food for two hours prior, but liquids are fine
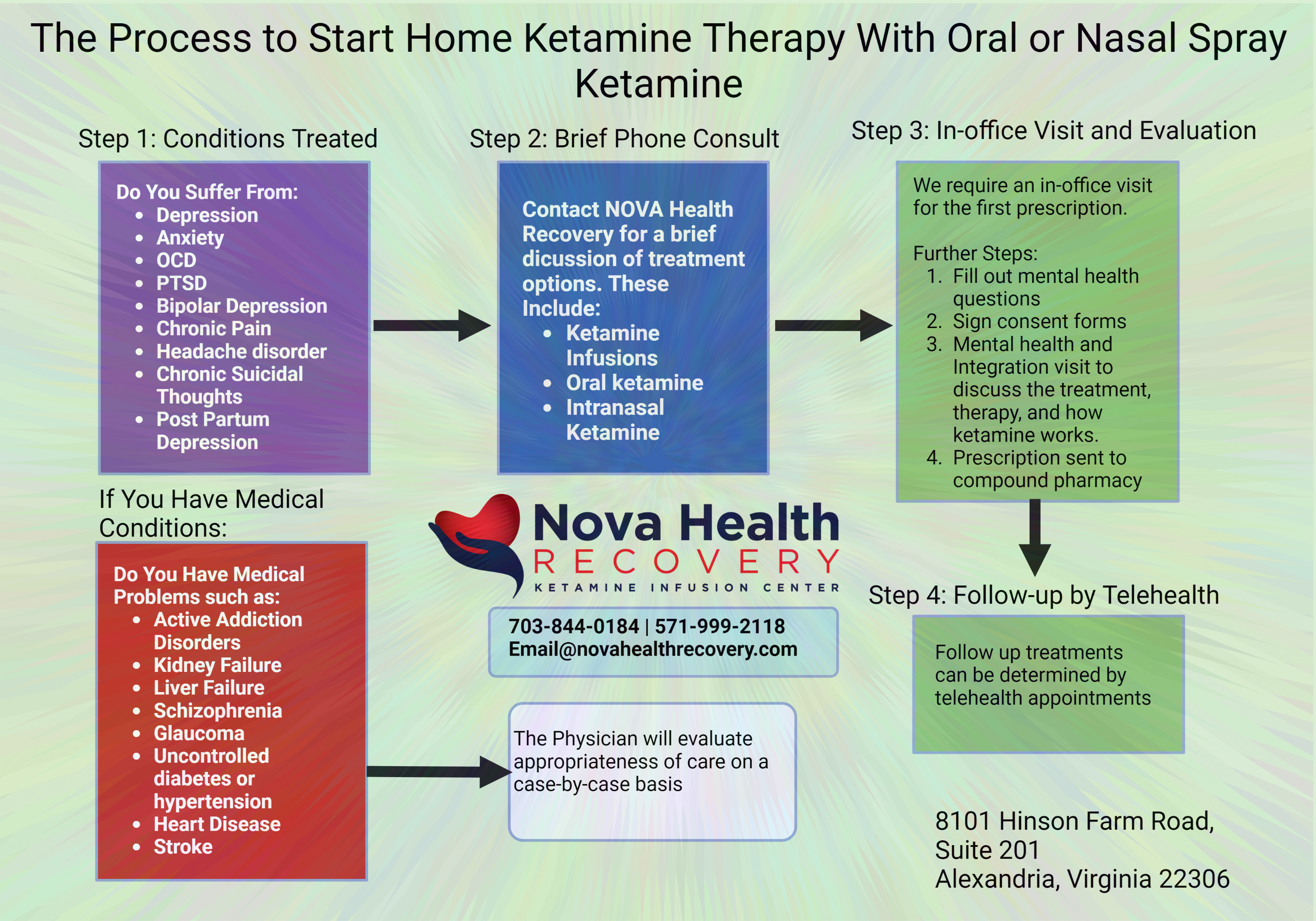
How about Ketamine Assisted Psychotherapy? Does NOVA Health Recovery Offer KAP Therapy?
What is Ketamine?
Ketamine is a dissociative anesthetic developed as a relative to PCP (phencyclidine) for the purposes of medical and veterinarian use. Dissociative anesthesia is the state of “lights on but nobody home,” in which the patient maintains airway reflexes while seemingly awake, yet they are completely unresponsive. The safety profile is such that it is one of the safest medications for the medical use and even the World Health Organization lists it as a ‘must have’ medication. In fact, per the W.H.O. worksheet, it (ketamine) does not require reliable electricity supply, oxygen, highly trained staff or monitoring systems to administer. That makes it critical in surgery in low- and middle-income countries.”
It was first synthesized in 1962, patented for use in 1966, and FDA approved for anesthesia in 1970. Ketamine could rapidly produce profound analgesia with a unique state of altered consciousness and a limited duration of effect that could be safely prolonged with repeated administration. A European Monitoring Centre for Drugs and Drug Addiction report identified 12 deaths in which ketamine was identified between 1987 and 2000, with three involving ketamine as the sole substance.

How does ketamine work?
Ketamine works in very complex ways in the brain and there is a lot of debate and unknown mechanisms that are at play. The details of its mechanisms of action are esoteric at best, but effectively Ketamine impacts numerous systems in the brain. Ketamine is an antagonist at the NMDA receptor site, which is involved with the neurotransmitter, glutamine, an excitatory neurotransmitter. Ketamine effectively binds to an area inside the receptor and blocks it from letting in excitatory ions, thus quieting the neuron. Ketamine works, in part, by activating certain neurons in a network and thereby shutting down other networks, resulting in an antidepressant effect. It also has a relaxant effect on airway smooth muscle that has been attributed to its inhibition of L-type voltage-dependent Ca2+ channels, which also may produce the altered perceptions and impaired verbal fluency during an infusion. It also blocks other systems in the brain such as preventing serotonin uptake and reducing pain perception. Ketamine’s block of large-conductance KCa channels (BK channels) preferentially suppresses spinal microglia hyperactivation after nerve injury and may explain its potent effects on neuropathic pain. Estrogen and progesterone may also potentiate the rapidity and potency of ketamine’s antidepressant effects, and hence there are sex differences in the response to ketamine.
Chronic stress, medical illness, alcohol, drugs, genetics, medications, toxins, and numerous other external traumatic interactions result in changes in the neurons of the brain with reduced synaptic connectivity. This occurs in the prefrontal cortex (involved with decision making and executive functioning) as well as in the hippocampus (the memory center). This can be seen on functional MRI’s as decreased activity and connectivity, and in fact, depression and mental illness can shrink these areas in size. That is where brain fog, decreased processing speed, and poor memory stem from. Cognitive tests demonstrate these phenomena, which results in poorer performance in the work and school environment as the individual is not fully able to think clearly due to these poorly connected memory and cognitive circuits. PTSD, anxiety, depression, and bipolar disorder all decrease functional connectivity in the brain.
Ketamine therapy has been shown to increase connectivity and repair nerves in the brain, and in fact the degree of clinical response is comparable to the degree of connectivity.
What are Neurons?
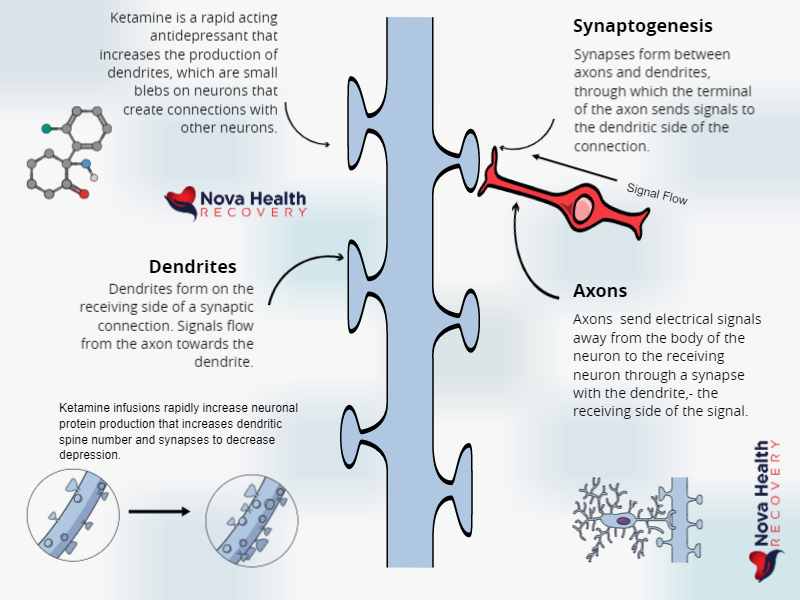
Neurons are the fundamental cells of the brain. The nerve cell body sends signals elsewhere through the axons and receives information through the dendrites. Dendrites are a bushy-like area of the nerve body that connects with other nerve cells, much like a cluster of ivy on a wall. These connections form the basis of learning and memory. When they are over-pruned, depression and other mental illnesses can result.

Health state – represented by a full ‘wall of ivy’ (neurons)
Over-pruned and depressed – fewer neurons and synapses – results in depression
The brain’s neural network is like a wall of ivy as in the first photo, where neurons are all interconnected. This pattern is lost and over pruned in depression, as in the lower photo. This results in vegetative, sickness behaviors such as low motivation, slow processing speed, poor memory, and no interest in otherwise rewarding events.
The brain keeps a balance between excitement and ‘rest’ through its neurotransmitters.
Neurotransmitters are small molecules that cross from one nerve cell to another. It is a way of communications, and the molecule type can help determine the message. Molecules such as dopamine, serotonin, norepinephrine, GABA, and Glutamate are examples of these neurotransmitters. The actions of these neurotransmitters are very regulated and too much excitatory or inhibitory transmitters can disrupt a balanced brain.
Glutamate is the most common excitatory neurotransmitter and is a key molecule in learning and neuroplasticity. Neuroplasticity is the ability of the brain to form new connections as in learning and forming new memories. Excess glutamate can damage nerve cells and this is associated with inflammation and depression.
Stress and neuronal damage
Stress with elevated cortisol levels results in damage to nerve endings as axons thin and dendrites disappear. Constant glutamate transmission from a brain on fire results in damage and loss of neurons. This is seen on MRI’s as measurable loss of brain volume. This is seen clinically as depression and anxiety. Depression is being recognized as more of a glutamate receptor issue. Ketamine can reverse this by replacing damaged neuronal spines and rapidly increasing connectivity in the brain.
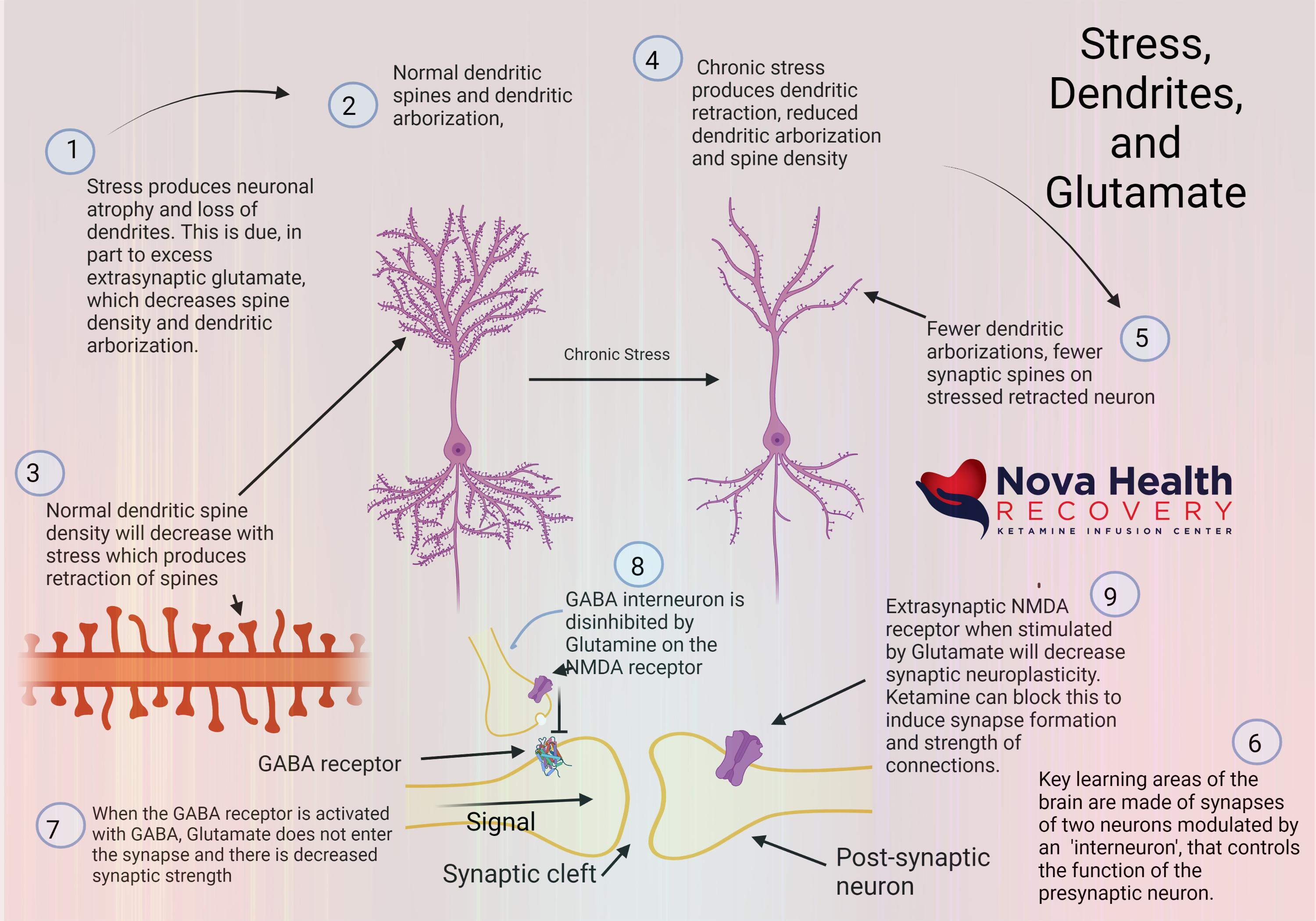
Ketamine rapidly allows neurons to form new spines
Ketamine and glutamate
Ketamine affects multiple receptors in the brain in complex manners. There are many different receptor types in the brain, some excitatory and others inhibitory, and ketamine interacts with many. In the case of glutamate, ketamine affects the NMDA receptor (N-methyl-D aspartate) receptor and the AMPA receptor., activating both.
Glutamate binds to NMDA receptors and activates the receptor to let calcium into the neuron, whereas when glutamate interacts with AMPA, it lets in sodium and lets out potassium from the neuron. This causes the activation of the nerve. Ketamine blocks the glutamate binding at the NMDA receptors of the postsynaptic cell (the neuron that receives the signal) but doesn’t block AMPA binding, with glutamate thus AMPA gets activated, which turns on the neuroplasticity machinery.
Brain-Derived Neurotrophic Factor (BDNF) is brain fertilizer
In summary, ketamine shifts activation by glutamate from the NMDA receptors to the AMPA receptors resulting in the production of BDNF, which promotes growth and survival of neurons and thereby produces neuroplasticity. In these same neurons, mTor (mammalian target of rapamycin) is activated, which synthesizes proteins involved in memory formation, particularly in the prefrontal cortex (the CEO of the brain) and the hippocampus (involved in memory). Thus, BDNF reverses the damage produced by chronic stress. This is what produces the new dendritic spines of learning and connection in the brain to reverse depression. This occurs within hours of an infusion.
Depression relief is all about the connectivity
Depression and other mood disorders disrupt connectivity in the brain. This can be seen as decreased activity on functional MRI’s as well as ‘brain shrinkage’ in key areas of the brain, such as the prefrontal cortex and hippocampus. This is seen at a microscopic level as decreased dendritic spines and retracted smaller neurons or even loss of neurons the results are brain fog, slow processing speed, weak memory, and symptoms of depression, such as hopelessness, lack of motivation, sadness, and many body-related symptoms. Ketamine represents a significant step forward in the rapid treatment and resolution of the damage to the brain caused by stress.
Add some content for each one of your videos, like a description, transcript or external links.To add, remove or edit tab names, go to Tabs.
Welcome to WordPress. This is your first post. Edit or delete it, then start writing!